Better coordination of systems, housing and income supports necessary to address mental illness and substance abuse in British Columbia
In response to the BC Government’s plans to build and implement a province-wide poverty reduction plan, CMHA BC Division has submitted a document outlining its recommendations it would like to see incorporated into this strategy. These 25 recommendations, have the potential to support British Columbians’ economic security, and by extension their mental health, well-being and recovery. The submission document can be accessed here.
Economic security is a key determinant of mental health and well-being. An adequate standard of living is a critical necessity to support the recovery of a person experiencing mental health or substance use-related illness.
“There is a complex two-way relationship between both mental health and substance use and poverty” says Kendra Milne, Senior Director of Policy, Planning & Government Relations at CMHA BC Division.
“People experiencing mental illness or substance use are at an increased risk of living in poverty because of stigma, discrimination, social exclusion, additional healthcare costs, and barriers to employment. Conversely, people living in poverty face an increased risk of experiencing stress and trauma, which has a strong correlation with mental illness and problematic substance use.”
The relationship between poverty, mental health and substance use is even more complex for people who experience additional forms of social exclusion or marginalization. For example, Indigenous people grappling with the impacts of inter-generational trauma and the ongoing consequences of colonization face disproportionate rates of poverty, mental illness and problematic substance use; the impacts of stigma, discrimination, cultural interference and poverty are deeply intertwined.
CMHA BC’s recommendations place an emphasis on creating a better coordination of systems, improved income supports and affordable and safe housing encompassing the following areas:
- Improved mental health and substance use services
- The need for cross-system coordination
- Income support
- Housing
- Employment
- Education
- Childcare
- Equity, cultural safety and trauma informed services
As BC develops its poverty reduction strategy, CMHA BC will continue to advocate for solutions that support mental health, wellbeing and recovery.
Notes to Editor:
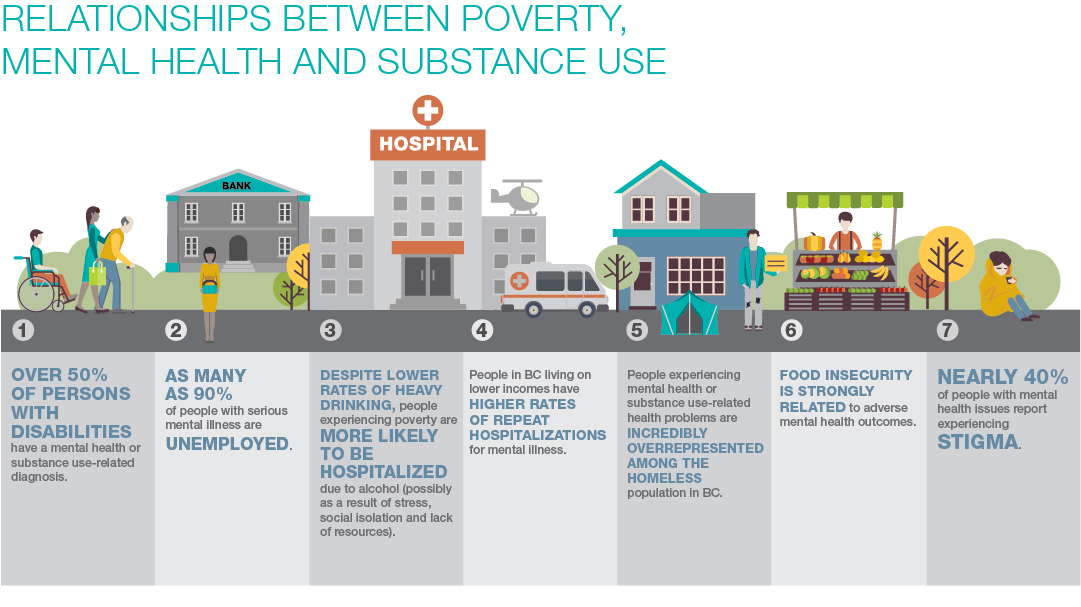
The consequences of the relationship between poverty, mental health and substance use are profound for people directly impacted:
- Over 50% of people designated as a “persons with disabilities” under the Employment and Assistance for Persons with Disabilities Act have a mental health or substance use-related diagnosis.[i] Many more are likely relying on regular income assistance.
- As many as 90% of people with serious mental illness are unemployed.[ii]
- Despite having lower rates of heavy drinking, people experiencing poverty are more likely to be hospitalized for reasons entirely connected to alcohol (possibly due to the increased stress, social isolation and lack of resources).[iii]
- People in BC living on lower incomes experience higher rates of repeat hospitalizations for mental illness.[iv]
- People experiencing mental health or substance use-related health problems are incredibly overrepresented among the homeless population in BC, which places them at increased risk for premature death.[v] In the context of incredibly low rental vacancy rates, people with mental health or substance use problems may be discriminated against in the provision of rental housing and face heightened insecurity.[vi]
- Food insecurity is tied strongly to adverse mental health outcomes.[vii]
- Nearly 40% of people with mental health issues report experiencing stigma, almost three times the rate of stigma experienced by those without mental health issues[viii] and people with substance use problems experience higher rates of stigma than those with any other health condition.[ix] Stigma not only undermines self-worth and health, but it also creates additional barriers to accessing services, employment, housing, and community/social supports.[x]
###
About the Canadian Mental Health Association (CMHA)
Celebrating our 100th anniversary in 2018, CMHA is Canada’s most established mental health charity and the nation-wide leader and champion for mental health. CMHA helps people access the resources they need to maintain and improve mental health, build resilience, and support recovery from mental illness. Each year in BC alone, CMHA serves more than 100,000 people all across the province. For mental health and addiction information and resources visit www.staging.cmha-bc.flywheelsites.com.
Media Contact
Lorna Allen, Communications Coordinator – Media, CMHA BC Division
P: 604-688-3234 ext. 6326
E: lorna.allen@cmha.bc.ca
[i] Data provided by the Ministry of Social Development and Poverty Reduction to the Supporting Increased Participation table.
[ii] Standing Committee on Human Resources, Skills and Social Development and the Status of Persons with Disabilities, Breaking the Cycle: A Study on Poverty Reduction (May 2017).
[iii] Canadian Institute for Health Information, Alcohol Harm in Canada:
Examining Hospitalizations Entirely Caused by Alcohol and Strategies to Reduce Alcohol Harm (2017).
[iv] Canadian Institute for Health Information, “Health Indicators Interactive Tool”, online: https://yourhealthsystem.cihi.ca/epub/ (searched using most recent year available, by province, for “30-day Readmission for Mental Illness”, “Mental Illness Hospitalization – T”, “Mental Illness Patient Days – T”, and “Patients with Repeat Hospitalizations for Mental Illness”).
[v] BC Non-Profit Housing Association and M. Thomson Consulting, 2017 Homeless Count in Metro Vancouver; Jessica Hannon, Dying on the Streets: Homeless Deaths in British Columbia, 2006-2015 (3rd Edition, 2017).
[vi] Greg Richmond, “Housing Our Homeless” Visions: BC’s Mental Health and Addiction Journal 12:3 (2017).
[vii] PROOF Food Insecurity Policy Research, “Fact Sheet: Food Insecurity and Mental Health” online: http://proof.utoronto.ca/resources/fact-sheets/#mentalhealth.
[viii] Jamie Livingston, Mental Illness-Related Structural Stigma: The Downward Spiral of Systemic Exclusion Final Report (Mental Health Commission of Canada, 2015).
[ix] Jamie Livingston et al, “The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review” Addiction 107:1 (2012).
[x] Supra footnote viii